Endometriosis Treatment
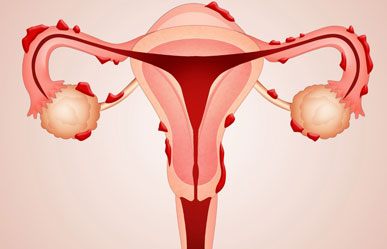
What is Endometriosis?
Endometriosis is a common gynecological condition where tissue similar to the lining of the uterus, called endometrium, grows outside the uterus. This abnormal growth can occur on the ovaries, fallopian tubes, outer surface of the uterus, and other organs in the pelvic region. Unlike the normal endometrium, this tissue has no way to exit the body during the menstrual cycle, leading to inflammation, scarring, and severe pain. Endometriosis can significantly affect a woman's quality of life, causing chronic pelvic pain, heavy menstrual bleeding, painful intercourse, and even infertility. Early diagnosis and proper treatment are essential to manage symptoms and improve overall reproductive health.
Symptoms of Endometriosis
The symptoms of endometriosis can vary from mild to severe and may differ from person to person. Some women may experience severe symptoms, while others may have minimal or no symptoms. Common symptoms of endometriosis include severe menstrual cramps (dysmenorrhea), chronic pelvic pain, pain during or after intercourse, heavy or irregular menstrual bleeding, pain during bowel movements or urination, and difficulty conceiving (infertility). Other symptoms may include fatigue, bloating, nausea, and lower back pain. The severity of pain does not necessarily correlate with the extent of the condition, meaning women with mild endometriosis can experience severe pain, while those with severe endometriosis may have minimal symptoms.
Causes of Endometriosis
The exact cause of endometriosis is not fully understood, but several factors are believed to contribute to its development. One of the primary theories is retrograde menstruation, where menstrual blood containing endometrial cells flows back through the fallopian tubes into the pelvic cavity instead of leaving the body. These endometrial cells then attach to the pelvic organs and grow. Other potential causes include hormonal imbalances, genetic predisposition, immune system disorders.
Lifestyle Changes to Manage Endometriosis
In addition to medical treatment, adopting certain lifestyle changes can help manage endometriosis symptoms effectively. Maintaining a balanced and anti-inflammatory diet rich in fruits, vegetables, whole grains, and omega-3 fatty acids can reduce inflammation and ease pain. Regular exercise and physical activity help improve blood circulation, reduce pelvic pain, and balance hormone levels. Stress management techniques such as yoga, meditation, and deep breathing can also alleviate chronic pain and emotional distress caused by endometriosis. Limiting the intake of processed foods, caffeine, and alcohol may help reduce inflammation and hormone imbalances associated with endometriosis.
When to See a Gynaecologist?
It is important to consult a gynecologist if you experience persistent pelvic pain, severe menstrual cramps, heavy or prolonged periods, painful intercourse, or difficulty conceiving. Early intervention and accurate diagnosis of endometriosis can help prevent complications and improve the chances of successful treatment. Women planning for pregnancy or experiencing severe endometriosis symptoms should not delay seeking medical care. The gynecologist will recommend personalized treatment options based on the severity of the condition and the patient’s reproductive goals. Managing endometriosis with the right medical care and lifestyle changes can significantly improve a woman’s health and quality of life.